
Is an Accident Policy Right for You?
Who Should Consider an Accident Insurance Policy? Life can be unpredictable, and even the most careful among us are not
Our health insurance blog is a trusted resource, keeping you informed and up-to-date on health insurance, health, and so much more.

Who Should Consider an Accident Insurance Policy? Life can be unpredictable, and even the most careful among us are not

Need Health Insurance for 2025? 31 States Have Extra Time to Sign Up to Start Coverage on 01/01/2025! Looking for
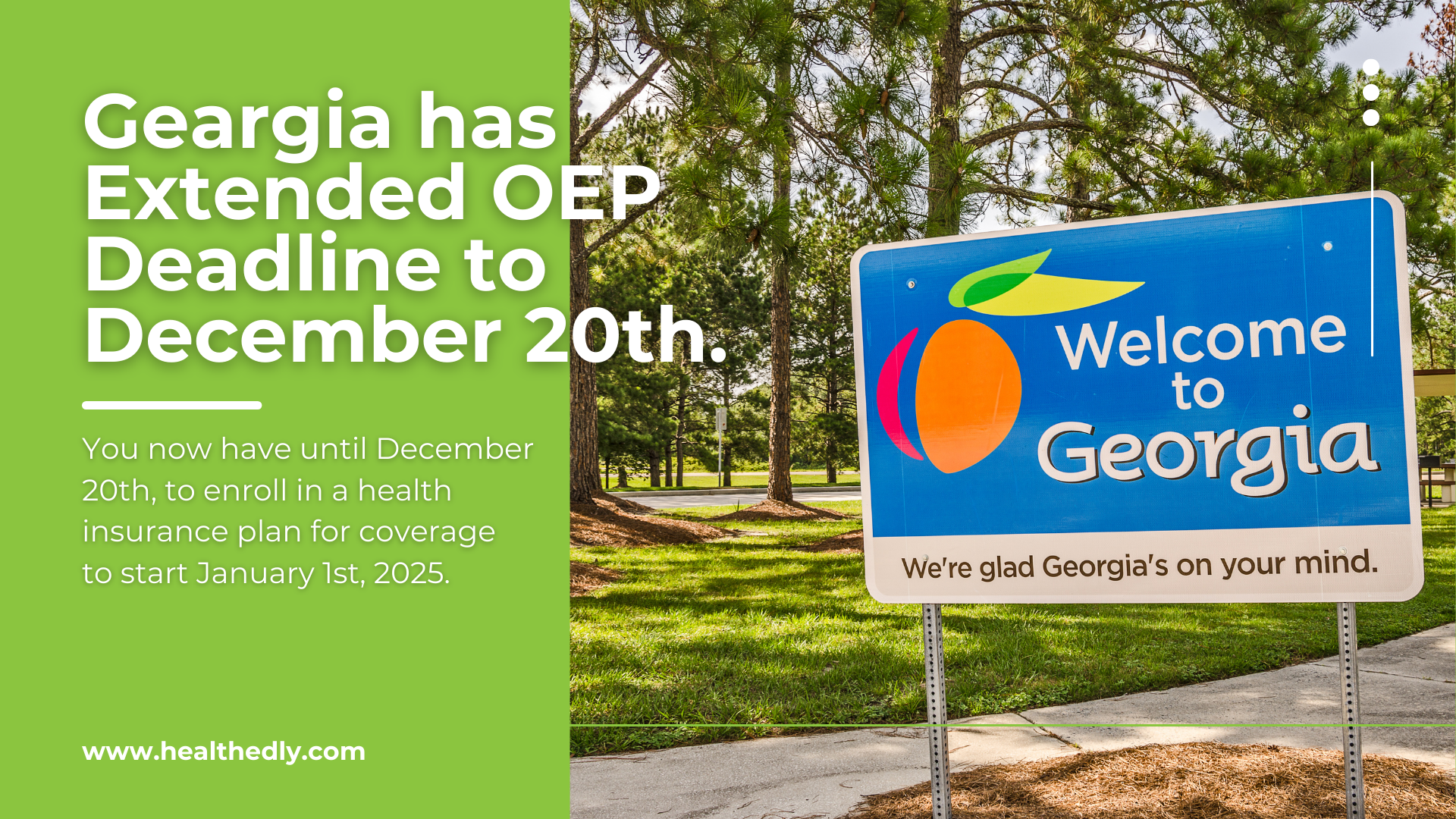
Great news for Georgia residents! The Georgia Access program has extended the deadline for January 1st health coverage, giving you more time to secure affordable health insurance for the new year.

As a private practice doctor, you’ve likely noticed an increase in patients—especially teens and young adults—who vape. While it’s marketed

If you’ve ever been to a concert, you know how thrilling the experience can be. The crowd’s energy, the lights,

Ever tried picking a health insurance plan and wondered what level you needed? With four options that offer lots of

Have you ever wondered why RSV causes so much concern among parents? It’s not just another sniffle. Respiratory syncytial virus,

Ah, the common cold—something we’ve all experienced and hope to avoid as much as possible. But when it hits, it

Welcoming your little one into the world is a beautiful experience, filled with joy, excitement, and yes, a few worries,

Accidents happen, and sometimes they leave us with cuts or wounds that need more than a bandage. But how do

Ever watched those late-night fitness products commercials and thought, “That looks great, but could I really do that?” If you’re

As a parent, have you ever found yourself standing in front of the drink aisle, staring at the endless options,







Healthedly Insurance Services, LLC all rights reserved. Healthedly.com is a non-government website that is owned and operated by Healthedly Insurance Services, LLC, which is a licensed health insurance agency. Healthedly Insurance Services, LLC is not affiliated with or endorsed by the U.S. government, Healthcare.gov or the deferral Medicare program. The purpose of this site is the solicitation of insurance. Contact may be made by an insurance agent/producer of the insurance company. We currently do not offer every plan available in your area. Healthedly Insurance Services, LLC currently represents 10 Medicare carriers, and 801 plans, and has access to plans in all 50 states plus the District of Columbia. Please contact Medicare.gov, 1-800-MEDICARE, or your local State Health insurance Program (SHIP) to get information on all of your options. Not all plans offer all of these benefits. Benefits may vary by carrier and location. Limitations and exclusions may apply. By using this site, you acknowledge that you have read and agree to our Privacy Policy, Do Not Call Policy, Terms of Service and SMS Terms & Conditions.




